Crohn's disease is an inflammatory bowel disease where chronic inflammation typically involves the lower part of the small intestine, the large intestine, or both and may affect any part of the digestive tract.
- Although the exact cause is unknown, an improperly functioning immune system may result in Crohn disease.
- Typical symptoms include chronic diarrhea (which sometimes is bloody), crampy abdominal pain, fever, loss of appetite, and weight loss.
- The diagnosis is based on a colonoscopy, video capsule endoscopy, and imaging tests such as barium x-rays, computed tomography, or magnetic resonance imaging.
- There is no cure for Crohn's disease.
- Treatment is aimed at relieving symptoms and reducing inflammation, but some people require surgery.
In the past few decades, Crohn's disease has become more common worldwide. However, it is most common among people of Northern European and Anglo-Saxon descent. It occurs about equally in both sexes, often runs in families, and seems to be more common among Ashkenazi Jews. Most people develop Crohn's disease before age 30, usually between the ages of 14 and 24.
Overview of Crohn Disease
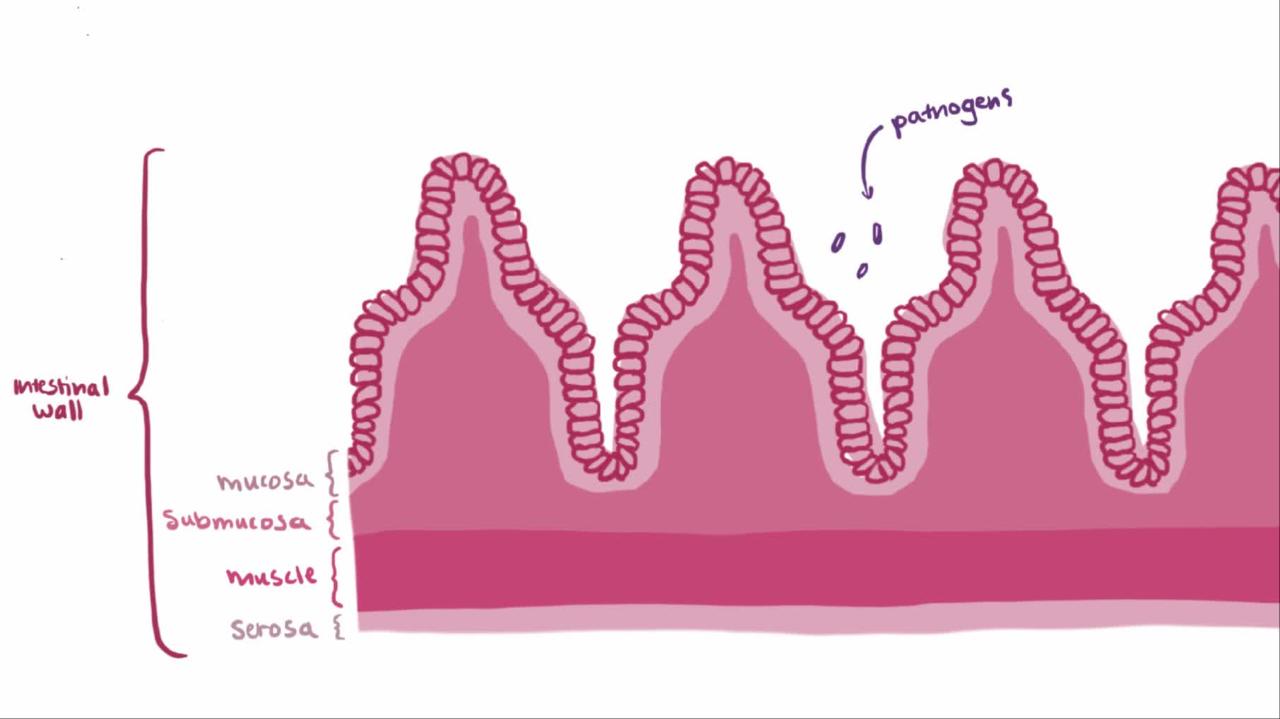
Most commonly, Crohn's disease occurs in the last portion of the small intestine (ileum) and in the large intestine, but it can occur in any part of the digestive tract, from the mouth to the anus and even in the skin around the anus. When Crohn's disease affects the colon, it is called Crohn colitis. Crohn's disease affects
- The small intestine alone (35% of people)
- The large intestine alone (20% of people)
- Both the last portion of the small intestine and the large intestine (45% of people)
The rectum is usually not affected, unlike in ulcerative colitis, in which the rectum is always involved. However, infections and other complications around the anus are not unusual. The disease may affect some segments of the intestinal tract while leaving normal segments (called skip areas) between the affected areas. Where Crohn's disease is active, the full thickness of the bowel is usually involved.

3D Model: Crohn Disease
The cause of Crohn's disease is not known for certain, but many researchers believe that a dysfunction of the immune system causes the intestine to overreact to an environmental, dietary, or infectious agent. Certain people may have a hereditary predisposition to this immune system dysfunction. Cigarette smoking seems to contribute to both the development and the periodic flare-ups (bouts or attacks) of Crohn disease. Oral contraceptives may increase the risk of Crohn disease.
For unclear reasons, people who have a higher socioeconomic status may have an increased risk of Crohn disease.
Several reports suggest that people who were breast-fed may be protected from developing inflammatory bowel disease.
Symptoms
The most common symptoms of Crohn's disease are
- Crampy abdominal pain
- Chronic diarrhea (which sometimes is bloody when the large intestine is severely affected)
- Fever
- Loss of appetite
- Weight loss
Symptoms of Crohn's disease may continue for days or weeks and may resolve without treatment. Complete and permanent recovery after a single attack is extremely rare. Crohn's disease almost always flares up at irregular intervals throughout a person's life. Flare-ups can be mild or severe, brief or prolonged. Severe flare-ups can lead to intense, constant pain, fever, and dehydration.
Why the symptoms come and go and what triggers new flare-ups or determines their severity is not known. Recurring inflammation tends to appear in the same area of the intestine, but it may spread to adjacent areas after a diseased segment has been removed surgically.
In children, abdominal pain and diarrhea often are not the main symptoms and may not appear at all. Instead, the main symptoms may be slow growth, joint inflammation (arthritis), fever, or weakness and fatigue resulting from anemia.
Complications
Complications of Crohn's disease include
- Intestinal blockage (obstruction)
- Perforation (rupture) of the bowel
- Abscesses (pus-filled pockets of infection) in the abdomen
- Fistulas (abnormal connecting channels between the intestine and skin or other organs)
- Anal fissures (tears in the skin of the anus) and anal abscesses
- Colon cancer (cancer of the large intestine)
Toxic megacolon is a rare complication that can happen when Crohn's disease affects the large intestine (colon). The large intestine stops its normal contractions and dilates, sometimes leading to peritonitis. People may need surgery.
Scarring due to chronic inflammation can cause intestinal blockage. Deep ulcers that penetrate through the bowel wall can create abscesses, open fistulas, or perforations. Fistulas may connect two different parts of the intestine. Fistulas may also connect the intestine and bladder or the intestine and the skin surface, especially around the anus. Although fistulas from the small intestine are common, wide-open holes (perforations) are rare. Fissures in the skin of the anus are common.

3D Model: Intestinal Fistulas

3D Model: Anorectal Fistula
When the large intestine is affected extensively by Crohn disease, rectal bleeding commonly occurs. After many years, the risk of colon cancer (cancer of the large intestine) is increased in people who have Crohn colitis. About one third of people who develop Crohn's disease have problems around the anus, especially fistulas and fissures in the lining of the mucus membrane of the anus.
Crohn's disease may lead to complications in other parts of the body. These complications include
- Gallstones
- Inadequate absorption of nutrients (malabsorption)
- Urinary tract infections
- Kidney stones
- Deposits of the protein amyloid in several organs (amyloidosis)
When Crohn's disease causes a flare-up of gastrointestinal symptoms, the person may also have the following:
- Inflammation of the joints (arthritis)
- Inflammation of the whites of the eyes (episcleritis)
- Mouth sores (aphthous stomatitis)
- Inflamed skin nodules on the arms and legs (erythema nodosum)
Even when Crohn's disease is not causing a flare-up of gastrointestinal symptoms, the person still may have the following entirely without relation to the bowel disease:
- Inflammation of the spine (ankylosing spondylitis)
- Inflammation of the pelvic joints (sacroiliitis)
- Inflammation inside the eye (uveitis)
- Inflammation of the bile ducts (primary sclerosing cholangitis)
- Dusky purple skin sores that may contain pus (pyoderma gangrenosum)
Diagnosis
- Blood and stool tests
- Imaging tests
- Colonoscopy
A doctor may suspect Crohn's disease in a person with recurring crampy abdominal pain and diarrhea, particularly if the person has a family history of Crohn's disease or a history of problems around the anus. Other clues to the diagnosis may include inflammation in the joints, eyes, or skin or stunted growth in a child. The doctor may feel a lump or fullness in the lower part of the abdomen, most often on the right side.
Blood and stool tests
No laboratory test specifically identifies Crohn disease, but blood tests may show anemia, abnormally high numbers of white blood cells, low levels of the protein albumin, and other indications of inflammation, such as an elevated erythrocyte sedimentation rate or level of C-reactive protein. A doctor may also do tests to determine how the liver is functioning.
If diarrhea is present, a doctor may collect stool samples to rule out certain infections.
Imaging tests
People who have severe abdominal pain and tenderness often have a computed tomography (CT) scan or magnetic resonance imaging (MRI) of their abdomen. CT or MRI may show a blockage, abscesses or fistulas, and other possible causes of inflammation of the abdomen (such as appendicitis).
People who have had symptoms that recur over a period of time may have x-rays taken of the stomach and small intestine after drinking liquid barium (called an upper gastrointestinal [GI] series) or have x-rays taken after receiving barium as an enema (called a barium enema). Newer approaches include CT enterography or magnetic resonance enterography. Another way in which the small intestine can be evaluated is with video capsule endoscopy.
Colonoscopy
People who have little pain and mostly diarrhea undergo a colonoscopy (an examination of the large intestine with a flexible viewing tube) and a biopsy (removal of a tissue specimen for microscopic examination). If Crohn's disease is limited to the small intestine, colonoscopy will not detect the disease unless the colonoscope is advanced all the way through the colon and into the last part of the small intestine where the inflammation most often resides.
Ulcer in Crohn DiseaseUlcer in Crohn Disease
Prognosis
Crohn's disease has no known cure and is characterized by intermittent flare-ups of symptoms. Flare-ups may be mild or severe, few or frequent. With proper treatment, most people continue to lead productive lives. However, about 10% of people are disabled by Crohn's disease and its complications.
Treatment
- Antidiarrheal drugs
- Aminosalicylates
- Corticosteroids
- Immunomodulating drugs
- Biologic agents
- Antibiotics
- Dietary regimens
- Sometimes surgery
Many treatments of Crohn's disease help reduce inflammation and relieve symptoms.
General management
Cramps and diarrhea may be relieved by taking loperamide or drugs that stop spasms in the abdomen (ideally before meals). Methylcellulose or psyllium preparations sometimes help prevent anal irritation by making the stool firmer. People should avoid eating fiber during flare-ups or if they have intestinal blockage.
Routine health maintenance measures, particularly vaccinations and cancer screening, are important.
Antidiarrheal drugs
These drugs, which may relieve cramps and diarrhea, include diphenoxylate, loperamide, deodorized opium tincture, and codeine. They are taken by mouth—preferably before meals.
Aminosalicylates
Aminosalicylates are drugs used to treat inflammation caused by inflammatory bowel disease. Sulfasalazine and related drugs such as mesalamine, olsalazine, and balsalazide are types of aminosalicylates. These drugs can suppress symptoms when they occur and reduce inflammation, especially in the large intestine. Typically these drugs are taken by mouth. Mesalamine is also available as a suppository or enema. Aminosalicylates do not work as well for relieving severe flare-ups.
Corticosteroids
Corticosteroids such as prednisone or prednisolone, which is given by mouth, may dramatically reduce fever and diarrhea, relieve abdominal pain and tenderness, and improve appetite and sense of well-being. However, long-term use of corticosteroids causes side effects (see Corticosteroids: Uses and Side Effects). Usually, high doses are taken initially to relieve major inflammation and symptoms caused by sudden flare-ups. The dose is then reduced and the drug is discontinued as soon as possible.
Another corticosteroid called budesonide has fewer side effects than prednisone, but it may not be quite as rapidly effective and usually does not prevent relapses beyond 6 months. Budesonide can be given by mouth or as an enema.
As with corticosteroids taken by mouth, the dose of corticosteroids taken in enema or foam form (such as hydrocortisone) is reduced and gradually stopped.
If the disease becomes severe, the person is hospitalized and corticosteroids are given by vein (intravenously).
Doctors give vitamin D and calcium supplements to all people who take corticosteroids.
Immunomodulating drugs
Azathioprine and mercaptopurine are drugs that decrease the actions of the immune system. They are effective for people with Crohn's disease who do not respond to other drugs and are especially effective for maintaining long periods of remission (periods of no symptoms). They significantly improve the person's overall condition, decrease the need for corticosteroids, and often heal fistulas. However, these drugs may not produce benefits for 1 to 3 months and may have potentially serious side effects.
The most common side effects of azathioprine and mercaptopurine are nausea, vomiting, and a general feeling of illness (malaise). A doctor closely monitors the person for other side effects such as allergic reactions, suppression of bone marrow (monitored by regularly measuring white blood cell counts), inflammation of the pancreas (pancreatitis), and sometimes liver problems. People who take these drugs have an increased risk of developing lymphoma, a cancer of white blood cells, and some types of skin cancer (monitored by routine skin examinations).
Blood tests that detect variations in one of the enzymes that metabolize azathioprine and mercaptopurine and that directly measure metabolite levels often help the doctor ensure safe and effective drug dosages.
Methotrexate, given by injection or by mouth once a week, often benefits people who do not respond to or who cannot tolerate corticosteroids, azathioprine, or mercaptopurine. Side effects include nausea, vomiting, hair loss, liver problems, kidney failure, and rarely lung problems. A low white blood cell count can also occur, and thus people taking methotrexate are susceptible to infection. Methotrexate is teratogenic (dangerous to a fetus) and hence not used in pregnancy. Both women and men taking methotrexate should make sure the female partner uses an effective contraceptive method (birth control) such as an intrauterine device (IUD), a contraceptive implant, or an oral contraceptive. Less effective methods of contraception, such as condoms, spermicides, diaphragms, cervical caps, and periodic abstinence, are discouraged. Doctors prescribe folic acid to decrease the side effects of methotrexate.
Cyclosporine is given by injection in high doses. This drug may help heal fistulas caused by Crohn disease, but it cannot safely be used long term because of side effects such as kidney problems, infections, and seizures.
Tacrolimus is given by mouth. This drug may help heal fistulas caused by Crohn disease. Side effects are similar to those of cyclosporine.
Biologic agents
Infliximab, which is derived from monoclonal antibodies to tumor necrosis factor (called a tumor necrosis factor inhibitor or TNF inhibitor), is another modifier of the immune system's actions. Infliximab is given as a series of infusions by vein. This drug can be given to treat moderate to severe Crohn's disease that has not responded to other drugs, to treat people with fistulas, and to maintain response when the disease is difficult to control.
Side effects that may occur with infliximab include worsening of an existing uncontrolled bacterial infection, reactivation of tuberculosis or hepatitis B, and an increase in the risk of some types of cancer. Some people have reactions such as fever, chills, nausea, headache, itching, or rash during the infusion (called infusion reactions). Before starting treatment with infliximab (or other TNF inhibitors such as adalimumab and certolizumab), people must be tested for tuberculosis and hepatitis B infection.
Adalimumab is a drug related to infliximab and also focuses on regulating the immune system. Adalimumab is given as a series of injections under the skin (subcutaneous injections) and so does not cause the possible infusion reactions of a drug given by vein such as infliximab. Adalimumab is particularly helpful for people who cannot tolerate or who no longer respond to infliximab. People may have pain and itching at the injection site.
Certolizumab is given as monthly subcutaneous injections. This drug works in a similar way as and causes side effects similar to those of infliximaband adalimumab.
Vedolizumab and natalizumab are drugs for people who have moderate to severe Crohn's disease that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect they cause is infection. Natalizumab is currently available only through a restricted-use program because it increases the risk of a fatal brain infection called progressive multifocal leukoencephalopathy (PML). Vedolizumab has a theoretical risk of PML because it is in the same class of drugs as natalizumab.
Ustekinumab is another kind of biologic agent. It is given as a series of infusions by vein or subcutaneous injections.
Broad-spectrum antibiotics and probiotics
Antibiotics that are effective against many types of bacteria are often prescribed. The antibiotic metronidazole is the most common choice for the treatment of abscesses and fistulas around the anus. Metronidazole may also help relieve the noninfectious symptoms of Crohn disease, such as diarrhea and abdominal cramps. However, when used for a long time, metronidazole can damage nerves, resulting in a pins-and-needles feeling in the arms and legs. This side effect usually disappears when the drug is stopped, but relapses of Crohn's disease after discontinuing metronidazole are common.
People should avoid consuming alcoholic beverages or products containing propylene glycol while taking metronidazole and should continue to avoid these substances for at least 3 days after metronidazole treatment is completed.
Some other antibiotics, such as ciprofloxacin or levofloxacin, may be used in place of or in combination with metronidazole. Rifaximin, a nonabsorbable antibiotic, is also sometimes used in treating active Crohn disease.
Some bacteria are naturally found in the body and promote the growth of good bacteria (probiotics). The daily use of probiotics, such as lactobacillus (typically present in yogurt), may be effective in preventing pouchitis (inflammation of a reservoir created during surgical removal of the large intestine and rectum).
Dietary regimens
Although some people claim that certain diets have helped improve their IBD, diets have not been shown to be effective in clinical trials. Nutritional therapy may help children grow more than they might otherwise, especially when given at nighttime by tube feeding. Occasionally, concentrated nutrients are given intravenously to compensate for the poor absorption of nutrients that is typical of Crohn disease.
Surgery
Most people with Crohn's disease require surgery at some point during their illness. Surgery is needed when the intestine is obstructed or when abscesses or fistulas do not heal. An operation to remove diseased sections of the intestine may relieve symptoms indefinitely, but it does not cure the disease. Crohn's disease tends to recur where the remaining intestine is rejoined, although several drug therapies initiated after surgery reduce this tendency.
A second operation is ultimately needed in nearly half of the people. Consequently, surgery is performed only if specific complications or the failure of drug treatment makes it necessary. Still, most people who have undergone surgery consider their quality of life to be better than it was before the operation.
Because smoking increases the risk of recurrence, especially in women, doctors encourage people to quit smoking.
General management
People who have severe disease may be hospitalized and given intravenous fluids to restore and maintain body fluids (hydration). Some people who have heavy rectal bleeding may require blood transfusions. People who have more chronic anemia may need iron supplements by mouth or intravenously.
Severity of symptoms
For people who have mild to moderate symptoms, mesalamine is typically the first drug of choice. Some doctors give antibiotics instead of mesalamine or give antibiotics to people who are not helped by mesalamine.
For people who have moderate to severe symptoms, corticosteroids (such as prednisone or budesonide) are given by mouth or vein.
People who are not helped by corticosteroids are given other drugs such as azathioprine, mercaptopurine, methotrexate, infliximab, adalimumab, vedolizumab, or certolizumab. A combination of these drugs may be given. These drugs help most people. If these drugs do not help,ustekinumab may be given.
If people have a blockage, doctors do nasogastric suction and give fluids by vein. In nasogastric suction, a tube is passed through the nose into the stomach or small intestine, and suction is applied to the tube to relieve abdominal swelling (distention).
For people whose symptoms developed suddenly or who have an abscess, fluids and antibiotics are given by vein in a hospital. Doctors drain the abscess surgically or by inserting a needle under the skin and drawing out the fluid.
Fistulas
People with fistulas around the anus (perianal fistulas) are given metronidazole and ciprofloxacin. If these drugs do not help people in 3 to 4 weeks, doctors may give azathioprine, mercaptopurine, or biologic agents. Cyclosporine is an alternative, but fistulas often recur after treatment. Tacrolimusmay help heal fistulas caused by Crohn disease. People may need definitive surgery to prevent the fistulas from recurring.
Maintenance regimens
To help keep symptoms from returning (that is, to maintain remission), people who require only an aminosalicylate or antibiotic to achieve remission can continue to take these drugs. People who were treated with a combination of azathioprine, mercaptopurine, methotrexate, or infliximab or adalimumab or certolizumab need to continue taking these drugs to maintain remission. People being treated with corticosteroids should have their doses gradually reduced. To maintain remission, they may need a combination of the drugs mentioned here.
During remission, doctors monitor people's symptoms and do blood tests. Routine x-rays or colonoscopy does not need to be done (except in people who have had Crohn's disease for 7 or 8 years or longer).

